Association of the Myocilin Gene Polymorphism With Primary Open Angle Glaucoma
Medical hypothesis discovery and innovation in ophthalmology,
Vol. 8 No. 1 (2019),
10 March 2019
,
Page 28-33
Abstract
Glaucoma is the second cause of irreversible blindness, and the Primary Open Angle Glaucoma (POAG) subtype is the most common type of glaucoma. It has been shown that genetic mutations increase the risk of POAG used for early detection. The aim of the current study was to determine the association between genetic variations of Myocilin (MYOC) gene and susceptibility to POAG in the Iranian population. This case-control study was conducted on patients with POAG, referred to Khatam-al Anbia Eye Hospital, Mashhad, Iran. The control group was selected from healthy patients with a refractive disorder, who had referred to this hospital. After extracting the DNA from the whole blood sample, the Polymerase Chain Reaction-Single-Strand Conformation Polymorphisms (PCR-SSCP) method was used to discriminate variability in sequences in three exons of MYOC gene locus, known as GLC1A. Clinical characteristics of the subjects, comprised of visual acuity, Cup to Disc Ratio (CDR), and Intra-Ocular Pressure (IOP) were statistically compared between the wild and mutant type of the MYOC gene using independent samples t-test, Chi-square, and logistic regression test with SPSS version 15.0 software. P-values of < 0.05 were considered significant. One hundred and forty participants (75.1% males) were studied in two groups of case (n = 70) and control (n = 70). The frequency of mutant alleles in patients and healthy groups was statistically significant (40% versus 11.5%, Odd’s Ratio (OR): 5.1, CI 95% for OR: 2.1 to 12.4, P-value < 0.001). Also, the detected mutation in the case group was significantly higher in exon 1 and 3 (15.7% versus 0%, P-value = 0.001, and 11.5% versus 2.8%, P-value = 0.049, respectively). Based on the result of the current study, it seems that the MYOC gene polymorphisms increased the risk of POAG in the Iranian population.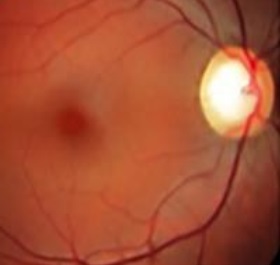
References
Quigley HA, Broman AT. The number of people with glaucoma worldwide in 2010 and 2020. Br J Ophthalmol. 2006;90(3):262-7. doi: 10.1136/bjo.2005.081224 pmid: 16488940
Kwon YH, Fingert JH, Kuehn MH, Alward WL. Primary open-angle glaucoma. N Engl J Med. 2009;360(11):1113-24. doi: 10.1056/NEJMra0804630 pmid: 19279343
Budde WM. Heredity in primary open-angle glaucoma. Curr Opin Ophthalmol. 2000;11(2):101-6. pmid: 10848214
Probert LA. A survey of hereditary glaucoma. Can Med Assoc J. 1952;66(6):563-8. pmid: 14945029
Havener WH. Chronic simple glaucoma: hereditary aspects. Am J Ophthalmol. 1955;40(6):828-31. pmid: 13268583
Francois J. Genetics and primary open-angle glaucoma. Am J Ophthalmol. 1966;61(4):652-65. pmid: 5931261
Fingert JH, Stone EM, Sheffield VC, Alward WL. Myocilin glaucoma. Surv Ophthalmol. 2002;47(6):547-61. pmid: 12504739
Alward WL. The genetics of open-angle glaucoma: the story of GLC1A and myocilin. Eye (Lond). 2000;14 ( Pt 3B):429-36. doi: 10.1038/eye.2000.127 pmid: 11026970
Souzeau E, Burdon KP, Dubowsky A, Grist S, Usher B, Fitzgerald JT, et al. Higher prevalence of myocilin mutations in advanced glaucoma in comparison with less advanced disease in an Australasian disease registry. Ophthalmology. 2013;120(6):1135-43. doi: 10.1016/j.ophtha.2012.11.029 pmid: 23453510
Elahi E, Narooie-Nejhad M, Suri F, Yazdani S. Myocilin mutations are not a major cause of primary congenital glaucoma in Iranian patients. J Ophthalmic Vis Res. 2010;5(2):101-4. pmid: 22737338
Caballero M, Rowlette LL, Borras T. Altered secretion of a TIGR/MYOC mutant lacking the olfactomedin domain. Biochim Biophys Acta. 2000;1502(3):447-60. pmid: 11068187
Sunnucks P, Wilson AC, Beheregaray LB, Zenger K, French J, Taylor AC. SSCP is not so difficult: the application and utility of single-stranded conformation polymorphism in evolutionary biology and molecular ecology. Mol Ecol. 2000;9(11):1699-710. pmid: 11091307
Suri F, Kalhor R, Zargar SJ, Nilforooshan N, Yazdani S, Nezari H, et al. Screening of common CYP1B1 mutations in Iranian POAG patients using a microarray-based PrASE protocol. Mol Vis. 2008;14(11):2349-56. pmid: 19096718
Graul TA, Kwon YH, Zimmerman MB, Kim CS, Sheffield VC, Stone EM, Alward WL. A case-control comparison of the clinical characteristics of glaucoma and ocular hypertensive patients with and without the myocilin Gln368Stop mutation. Am J Ophthalmol. 2002 Dec;134(6):884-90. pmid: 12470758
Craig JE, Baird PN, Healey DL, McNaught AI, McCartney PJ, Rait JL, et al. Evidence for genetic heterogeneity within eight glaucoma families, with the GLC1A Gln368STOP mutation being an important phenotypic modifier. Ophthalmology. 2001;108(9):1607-20. pmid: 11535458
- Abstract Viewed: 1288 times
- Full Text PDF Downloaded: 899 times


