Sight-threatening ocular manifestations in the post-coronavirus pandemic era
Medical hypothesis, discovery & innovation in optometry,
Vol. 6 No. 4 (2025),
30 January 2026
,
Page 181-195
https://doi.org/10.51329/mehdioptometry238
Abstract
Background: Coronavirus disease (COVID-19) infection can be associated with post-recovery sight-threatening complications like optic neuritis, retinal vascular occlusions, endophthalmitis, and panophthalmitis. This study was conducted to explore the various sight-threatening post-COVID-19 ophthalmic manifestations.Methods: This retrospective observational case series included seven patients who were diagnosed with sight-threatening manifestations post-COVID-19. They underwent detailed ophthalmic and systemic evaluation, including laboratory investigations for systemic hypercoagulable and inflammatory markers.
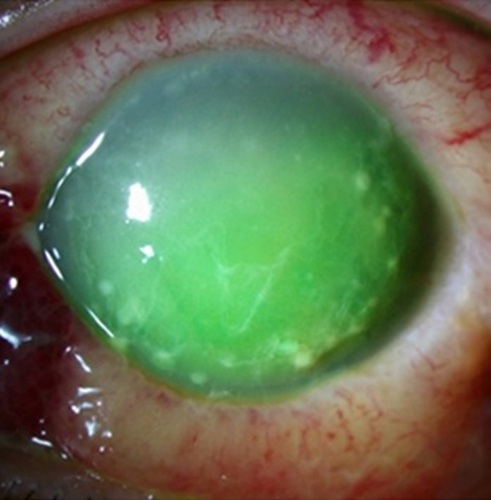
Results: Seven Indian patients (6 males:1 female, age range 37–66 years) presented to us with severe eye pain, acute loss of vision, redness, and watering after being diagnosed and treated for COVID-19 infection. The time from COVID-19 diagnosis to ocular sampling was 14–60 days (median 27), that of ocular symptoms to ocular sampling 1–50 days (median 4). Visual acuity ranged from no perception of light to 20/36. Three patients were pre-existing diabetics, two developed diabetes during their COVID-19 treatment. Diagnosis included one case of central retinal artery occlusion, one case of vitreous hemorrhage with retinal vasculitis, two cases of presumed bacterial endogenous endophthalmitis, one case of presumed fungal endophthalmitis, and two cases of panophthalmitis, one of them bilateral. Patients with infective intraocular inflammation were subjected to blood, ocular specimens, and urine cultures, which yielded growth in some patients. PCR of ocular specimens were positive for panfungal and/or eubacterial genome. Treatment included oral and systemic antimicrobial therapy with or without systemic steroids, with intravitreal antibiotics and/or steroids in selected cases. Final visual outcome ranged from no perception of light to 20/20.
Conclusions: Patients in this group had both vascular occlusions and infection as a cause of sight-threatening visual loss. Functional visual outcome may not be achieved in this diverse group of patients. Multi-specialty management was required in most of the cases. Larger prospective studies with controls are required to clarify pathogenesis, optimal screening, and management strategies for post-COVID-19 ocular complications.
Keywords:
- coronavirus disease 2019
- COVID 19
- central retinal artery occlusion
- vasculitides
- infectious endophthalmitides
- panophthalmitides
References
1. Wu P, Duan F, Luo C, Liu Q, Qu X, Liang L, Wu K. Characteristics of Ocular Findings of Patients With Coronavirus Disease 2019 (COVID-19) in Hubei Province, China. JAMA Ophthalmol. 2020 May 1;138(5):575-578. doi: 10.1001/jamaophthalmol.2020.1291. PMID: 32232433; PMCID: PMC7110919.
2. Acharya S, Diamond M, Anwar S, Glaser A, Tyagi P. Unique case of central retinal artery occlusion secondary to COVID-19 disease. IDCases. 2020;21:e00867. doi: 10.1016/j.idcr.2020.e00867. Epub 2020 Jun 18. PMID: 32572363; PMCID: PMC7301806.
3. Insausti-García A, Reche-Sainz JA, Ruiz-Arranz C, López Vázquez Á, Ferro-Osuna M. Papillophlebitis in a COVID-19 patient: Inflammation and hypercoagulable state. Eur J Ophthalmol. 2022 Jan;32(1):NP168-NP172. doi: 10.1177/1120672120947591. Epub 2020 Jul 30. PMID: 32735134; PMCID: PMC7399568.
4. Landecho MF, Yuste JR, Gándara E, Sunsundegui P, Quiroga J, Alcaide AB, García-Layana A. COVID-19 retinal microangiopathy as an in vivo biomarker of systemic vascular disease? J Intern Med. 2021 Jan;289(1):116-120. doi: 10.1111/joim.13156. Epub 2020 Jul 30. PMID: 32729633.
5. Dumitrascu OM, Volod O, Bose S, Wang Y, Biousse V, Lyden PD. Acute ophthalmic artery occlusion in a COVID-19 patient on apixaban. J Stroke Cerebrovasc Dis. 2020 Aug;29(8):104982. doi: 10.1016/j.jstrokecerebrovasdis.2020.104982. Epub 2020 May 23. PMID: 32689586; PMCID: PMC7245224.
6. Ortiz-Seller A, Martínez Costa L, Hernández-Pons A, Valls Pascual E, Solves Alemany A, Albert-Fort M. Ophthalmic and Neuro-ophthalmic Manifestations of Coronavirus Disease 2019 (COVID-19). Ocul Immunol Inflamm. 2020 Nov 16;28(8):1285-1289. doi: 10.1080/09273948.2020.1817497. Epub 2020 Oct 6. PMID: 33021422.
7. Sanjay S, Srinivasan P, Jayadev C, Mahendradas P, Gupta A, Kawali A, Shetty R. Post COVID-19 Ophthalmic Manifestations in an Asian Indian Male. Ocul Immunol Inflamm. 2021 May 19;29(4):656-661. doi: 10.1080/09273948.2020.1870147. Epub 2021 Mar 18. PMID: 33733987.
8. Sanjay S, Gowda PB, Rao B, Mutalik D, Mahendradas P, Kawali A, Shetty R. "Old wine in a new bottle" - post COVID-19 infection, central serous chorioretinopathy and the steroids. J Ophthalmic Inflamm Infect. 2021 May 14;11(1):14. doi: 10.1186/s12348-021-00244-4. PMID: 33987731; PMCID: PMC8118683.
9. Sanjay S, Mutalik D, Gowda S, Mahendradas P, Kawali A, Shetty R. "Post Coronavirus Disease (COVID-19) Reactivation of a Quiescent Unilateral Anterior Uveitis". SN Compr Clin Med. 2021;3(9):1843-1847. doi: 10.1007/s42399-021-00985-2. Epub 2021 Jun 7. PMID: 34124585; PMCID: PMC8184259.
10. Sanjay S, Kawali A, Mahendradas P, Shetty B. Post Coronavirus Disease (COVID)-19 Disease and Unilateral Visual Impairment. Curr Eye Res. 2021 Dec;46(12):1938. doi: 10.1080/02713683.2021.1905001. Epub 2021 Mar 25. PMID: 33729900.
11. Mahendradas P, Hande P, Patil A, Kawali A, Sanjay S, Ahmed SA, Thomas S, Shetty R. Bilateral Post Fever Retinitis With Retinal Vascular Occlusions Following Severe Acute Respiratory Syndrome Corona Virus (SARS-CoV2) Infection. Ocul Immunol Inflamm. 2022 Oct-Nov;30(7-8):1715-1720. doi: 10.1080/09273948.2021.1936564. Epub 2021 Jul 6. PMID: 34228600.
12. Sanjay S, Agrawal S, Jayadev C, Kawali A, Gowda PB, Shetty R, Mahendradas P. Posterior segment manifestations and imaging features post-COVID-19. Med Hypothesis Discov Innov Ophthalmol. 2021 Nov 17;10(3):95-106. doi: 10.51329/mehdiophthal1427. PMID: 37641707; PMCID: PMC10460223.
13. Sanjay S, Rao VK, Mutalik D, Mahendradas P, Kawali A, Shetty R. Post corona virus Disease-19 (COVID-19): Hyper inflammatory syndrome-associated bilateral anterior uveitis and multifocal serous retinopathy secondary to steroids. Indian Journal of Rheumatology. 2021 Oct 1;16(4):451-5. doi: 10.4103/injr.injr_330_20.
14. Sanjay S, Singh YP, Roy D, Mahendradas P, Kawali A, Shetty R. Recurrent bilateral idiopathic anterior uveitis with vitritis post Coronavirus Disease 2019 infection. Indian Journal of Rheumatology. 2021 Dec;16(4):460-3. doi: 10.4103/injr.injr_114_21.
15. Sanjay S, Kawali A, Agrawal S, Mahendradas P. Unilateral acute anterior sclero-uveitis preceding Corona virus disease (COVID-19). The Pan-American Journal of Ophthalmology. 2022 Jan 1;4(1):26. doi: 10.4103/pajo.pajo_14_22.
16. Sanjay S, Bhakti Mistra S, Patro SK, Kawali A, Shetty R, Mahendradas P. Systemic Markers in Ophthalmic Manifestations of Post Corona Virus Disease-19 (COVID-19). Ocul Immunol Inflamm. 2023 Feb;31(2):410-415. doi: 10.1080/09273948.2021.2025253. Epub 2022 Feb 9. PMID: 35138993.
17. Sanjay S, Poornachandra B, Kawali A, Shetty R, Narayana VC, Agrawal S, Mahendradas P. Unilateral Endogenous Bacterial Endophthalmitis Post-Coronavirus Disease-19 in an Healthy Asian Indian Male. Beyoglu Eye J. 2022 Aug 5;7(3):240-246. doi: 10.14744/bej.2022.94546. PMID: 36185987; PMCID: PMC9522998.
18. Jabs DA, Nussenblatt RB, Rosenbaum JT; Standardization of Uveitis Nomenclature (SUN) Working Group. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005 Sep;140(3):509-16. doi: 10.1016/j.ajo.2005.03.057. PMID: 16196117; PMCID: PMC8935739.
19. Nussenblatt RB, Palestine AG, Chan CC, Roberge F. Standardization of vitreal inflammatory activity in intermediate and posterior uveitis. Ophthalmology. 1985 Apr;92(4):467-71. doi: 10.1016/s0161-6420(85)34001-0. PMID: 4000641.
20. Forget P, Khalifa C, Defour JP, Latinne D, Van Pel MC, De Kock M. What is the normal value of the neutrophil-to-lymphocyte ratio? BMC Res Notes. 2017 Jan 3;10(1):12. doi: 10.1186/s13104-016-2335-5. PMID: 28057051; PMCID: PMC5217256.
21. Arabska J, ?ucka A, Magierski R, Sobów T, Wysoki?ski A. Neutrophil-lymphocyte ratio is increased in elderly patients with first episode depression, but not in recurrent depression. Psychiatry Res. 2018 May;263:35-40. doi: 10.1016/j.psychres.2018.02.043. Epub 2018 Feb 21. PMID: 29490259.
22. Prokop M, van Everdingen W, van Rees Vellinga T, Quarles van Ufford H, Stöger L, Beenen L, Geurts B, Gietema H, Krdzalic J, Schaefer-Prokop C, van Ginneken B, Brink M; COVID-19 Standardized Reporting Working Group of the Dutch Radiological Society. CO-RADS: A Categorical CT Assessment Scheme for Patients Suspected of Having COVID-19-Definition and Evaluation. Radiology. 2020 Aug;296(2):E97-E104. doi: 10.1148/radiol.2020201473. Epub 2020 Apr 27. PMID: 32339082; PMCID: PMC7233402.
23. Elmokadem AH, Mounir AM, Ramadan ZA, Elsedeiq M, Saleh GA. Comparison of chest CT severity scoring systems for COVID-19. Eur Radiol. 2022 May;32(5):3501-3512. doi: 10.1007/s00330-021-08432-5. Epub 2022 Jan 15. PMID: 35031841; PMCID: PMC8760133.
24. Merli G, Spiro TE, Olsson CG, Abildgaard U, Davidson BL, Eldor A, Elias D, Grigg A, Musset D, Rodgers GM, Trowbridge AA, Yusen RD, Zawilska K; Enoxaparin Clinical Trial Group. Subcutaneous enoxaparin once or twice daily compared with intravenous unfractionated heparin for treatment of venous thromboembolic disease. Ann Intern Med. 2001 Feb 6;134(3):191-202. doi: 10.7326/0003-4819-134-3-200102060-00009. PMID: 11177331.
25. Cerfolio RJ, Bryant AS, Thurber JS, Bass CS, Lell WA, Bartolucci AA. Intraoperative solumedrol helps prevent postpneumonectomy pulmonary edema. Ann Thorac Surg. 2003 Oct;76(4):1029-33; discussion 1033-5. doi: 10.1016/s0003-4975(03)00879-8. PMID: 14529979.
26. Billett HH, Reyes-Gil M, Szymanski J, Ikemura K, Stahl LR, Lo Y, Rahman S, Gonzalez-Lugo JD, Kushnir M, Barouqa M, Golestaneh L, Bellin E. Anticoagulation in COVID-19: Effect of Enoxaparin, Heparin, and Apixaban on Mortality. Thromb Haemost. 2020 Dec;120(12):1691-1699. doi: 10.1055/s-0040-1720978. Epub 2020 Nov 13. PMID: 33186991; PMCID: PMC7869055.
27. Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, Nigoghossian C, Ageno W, Madjid M, Guo Y, Tang LV, Hu Y, Giri J, Cushman M, Quéré I, Dimakakos EP, Gibson CM, Lippi G, Favaloro EJ, Fareed J, Caprini JA, Tafur AJ, Burton JR, Francese DP, Wang EY, Falanga A, McLintock C, Hunt BJ, Spyropoulos AC, Barnes GD, Eikelboom JW, Weinberg I, Schulman S, Carrier M, Piazza G, Beckman JA, Steg PG, Stone GW, Rosenkranz S, Goldhaber SZ, Parikh SA, Monreal M, Krumholz HM, Konstantinides SV, Weitz JI, Lip GYH; Global COVID-19 Thrombosis Collaborative Group, Endorsed by the ISTH, NATF, ESVM, and the IUA, Supported by the ESC Working Group on Pulmonary Circulation and Right Ventricular Function. COVID-19 and Thrombotic or Thromboembolic Disease: Implications for Prevention, Antithrombotic Therapy, and Follow-Up: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020 Jun 16;75(23):2950-2973. doi: 10.1016/j.jacc.2020.04.031. Epub 2020 Apr 17. PMID: 32311448; PMCID: PMC7164881.
28. Bapaye MM, Nair AG, Bapaye CM, Bapaye MM, Shukla JJ. Simultaneous Bilateral Central Retinal Artery Occlusion following COVID-19 Infection. Ocul Immunol Inflamm. 2021 May 19;29(4):671-674. doi: 10.1080/09273948.2021.1891262. Epub 2021 Apr 15. PMID: 33856275.
29. Erdem S, Karahan M, Dursun ME, Ava S, Hazar L, Katran I, Keklikci U. Retinal Vasculitis Case Developing in the Early Period after COVID-19. Klin Monbl Augenheilkd. 2022 Sep;239(9):1132-1133. English. doi: 10.1055/a-1363-1326. Epub 2021 Apr 14. PMID: 33853180.
30. Seah I, Agrawal R. Can the Coronavirus Disease 2019 (COVID-19) Affect the Eyes? A Review of Coronaviruses and Ocular Implications in Humans and Animals. Ocul Immunol Inflamm. 2020 Apr 2;28(3):391-395. doi: 10.1080/09273948.2020.1738501. Epub 2020 Mar 16. PMID: 32175797; PMCID: PMC7103678.
31. Hooks JJ, Percopo C, Wang Y, Detrick B. Retina and retinal pigment epithelial cell autoantibodies are produced during murine coronavirus retinopathy. J Immunol. 1993 Sep 15;151(6):3381-9. PMID: 8397257.
32. Becker RC. COVID-19 update: Covid-19-associated coagulopathy. J Thromb Thrombolysis. 2020 Jul;50(1):54-67. doi: 10.1007/s11239-020-02134-3. PMID: 32415579; PMCID: PMC7225095.
33. Sen S, Kannan NB, Kumar J, Rajan RP, Kumar K, Baliga G, Reddy H, Upadhyay A, Ramasamy K. Retinal manifestations in patients with SARS-CoV-2 infection and pathogenetic implications: a systematic review. Int Ophthalmol. 2022 Jan;42(1):323-336. doi: 10.1007/s10792-021-01996-7. Epub 2021 Aug 11. PMID: 34379290; PMCID: PMC8356207.
34. Tao DL, Bien JY, DeLoughery TG, Shatzel JJ. Extended thromboprophylaxis with direct oral anticoagulants for medical patients: a systematic review and meta-analysis. Blood. 2017 Feb 2;129(5):653-655. doi: 10.1182/blood-2016-10-747931. Epub 2016 Dec 20. PMID: 27998890.
35. Pinto AA, Carroll LS, Nar V, Varatharaj A, Galea I. CNS inflammatory vasculopathy with antimyelin oligodendrocyte glycoprotein antibodies in COVID-19. Neurol Neuroimmunol Neuroinflamm. 2020 Jun 10;7(5):e813. doi: 10.1212/NXI.0000000000000813. PMID: 32522768; PMCID: PMC7309522.
36. Roncati L, Ligabue G, Fabbiani L, Malagoli C, Gallo G, Lusenti B, Nasillo V, Manenti A, Maiorana A. Type 3 hypersensitivity in COVID-19 vasculitis. Clin Immunol. 2020 Aug;217:108487. doi: 10.1016/j.clim.2020.108487. Epub 2020 May 29. PMID: 32479986; PMCID: PMC7256503.
37. Xie CA, Singh J, Tyagi M, Androudi S, Dave VP, Arora A, Gupta V, Agrawal R, Mi H, Sen A. Endogenous Endophthalmitis - A Major Review. Ocul Immunol Inflamm. 2023 Sep;31(7):1362-1385. doi: 10.1080/09273948.2022.2126863. Epub 2022 Oct 28. PMID: 36306406.
38. Cunningham ET, Flynn HW, Relhan N, Zierhut M. Endogenous Endophthalmitis. Ocul Immunol Inflamm. 2018;26(4):491-495. doi: 10.1080/09273948.2018.1466561. PMID: 29768116; PMCID: PMC6448583.
39. Ren C, Li Z, Meng F, Du Y, Sun H, Guo B. Endogenous endophthalmitis caused by urinary tract infection: A case report. Medicine (Baltimore). 2023 Nov 17;102(46):e36139. doi: 10.1097/MD.0000000000036139. PMID: 37986372; PMCID: PsMC10659675.
40. Shroff D, Narula R, Atri N, Chakravarti A, Gandhi A, Sapra N, Bhatia G, Pawar SR, Narain S. Endogenous fungal endophthalmitis following intensive corticosteroid therapy in severe COVID-19 disease. Indian J Ophthalmol. 2021 Jul;69(7):1909-1914. doi: 10.4103/ijo.IJO_592_21. PMID: 34146056; PMCID: PMC8374784.
41. Obata R, Maeda T, Rizk D, Kuno T. Increased Secondary Infection in COVID-19 Patients Treated with Steroids in New York City. Jpn J Infect Dis. 2021 Jul 21;74(4):307-315. doi: 10.7883/yoken.JJID.2020.884. Epub 2020 Dec 25. PMID: 33390434.
42. Agarwal M, Sachdeva M, Pal S, Shah H, Kumar R M, Banker A. Endogenous Endophthalmitis A Complication of COVID-19 Pandemic: A Case Series. Ocul Immunol Inflamm. 2021 May 19;29(4):726-729. doi: 10.1080/09273948.2021.1945111. Epub 2021 Jul 13. PMID: 34255587.
43. Bilgic A, Sudhalkar A, Gonzalez-Cortes JH, March de Ribot F, Yogi R, Kodjikian L, Mathis T. ENDOGENOUS ENDOPHTHALMITIS IN THE SETTING OF COVID-19 INFECTION: A Case Series. Retina. 2021 Aug 1;41(8):1709-1714. doi: 10.1097/IAE.0000000000003168. PMID: 33734193.
44. Verma S, Walinjkar JA. A case of endogenous endophthalmitis in COVID-19 pandemic. Apollo Medicine. 2020 Sep;17(3):229-32. doi: https://journals.sagepub.com/doi/abs/10.4103/am.am_71_20.
45. Shah KK, Venkatramani D, Majumder PD. A case series of presumed fungal endogenous endophthalmitis in post COVID-19 patients. Indian J Ophthalmol. 2021 May;69(5):1322-1325. doi: 10.4103/ijo.IJO_3755_20. PMID: 33913891; PMCID: PMC8186646.
46. Khatwani PR, Goel NP, Trivedi KY, Aggarwal SV. Unveiling endophthalmitis post COVID-19 - A case series. Indian J Ophthalmol. 2021 Oct;69(10):2869-2871. doi: 10.4103/ijo.IJO_1616_21. PMID: 34571655; PMCID: PMC8597453.
47. Abdelkader MFSO, Elshafei AMK, Nassar MM, Abu Elela MA, Abdallah RMA. Combined endophthalmitis and orbital cellulitis in patients with corona virus disease (COVID-19). J Ophthalmic Inflamm Infect. 2021 Sep 15;11(1):27. doi: 10.1186/s12348-021-00258-y. PMID: 34523045; PMCID: PMC8440116.
48. Jain M, Brar AS, Rath S, Kelgaokar A, Behera HS. Fulminant fungal endogenous endophthalmitis following SARS-CoV-2 infection: A case report. Indian J Ophthalmol. 2022 May;70(5):1819-1821. doi: 10.4103/ijo.IJO_1951_21. PMID: 35502083; PMCID: PMC9333037.
49. Deepa MJ, Megharaj C, Patil S, Rani PK. Cryptococcus laurentii endogenous endophthalmitis post COVID-19 infection. BMJ Case Rep. 2022 May 11;15(5):e246637. doi: 10.1136/bcr-2021-246637. PMID: 35545307; PMCID: PMC9096502.
50. Sahu ES, Lahoti K, Bhargava A, Subhedar V, Sahu A. Subretinal Aspergillus Abscess in Post COVID-19 Recovered Patients - An Emerging Problem. Ocul Immunol Inflamm. 2023 Jan;31(1):127-133. doi: 10.1080/09273948.2021.1993271. PMID: 34784260.
51. Song M, Graubard BI, Rabkin CS, Engels EA. Neutrophil-to-lymphocyte ratio and mortality in the United States general population. Sci Rep. 2021 Jan 11;11(1):464. doi: 10.1038/s41598-020-79431-7. PMID: 33431958; PMCID: PMC7801737.
52. Kurtul BE, Ozer PA. Neutrophil-to-lymphocyte ratio in ocular diseases: a systematic review. Int J Ophthalmol. 2019 Dec 18;12(12):1951-1958. doi: 10.18240/ijo.2019.12.18. PMID: 31850181; PMCID: PMC6901879.
53. Ozgonul C, Sertoglu E, Mumcuoglu T, Kucukevcilioglu M. Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio as Novel Biomarkers of Primary Open-Angle Glaucoma. J Glaucoma. 2016 Oct;25(10):e815-e820. doi: 10.1097/IJG.0000000000000392. PMID: 26918914.
54. Chittawar S, Dutta D, Qureshi Z, Surana V, Khandare S, Dubey TN. Neutrophil-lymphocyte Ratio is a Novel Reliable Predictor of Nephropathy, Retinopathy, and Coronary Artery Disease in Indians with Type-2 Diabetes. Indian J Endocrinol Metab. 2017 Nov-Dec;21(6):864-870. doi: 10.4103/ijem.IJEM_197_17. PMID: 29285450; PMCID: PMC5729675.
55. Ulu SM, Dogan M, Ahsen A, Altug A, Demir K, Acartürk G, Inan S. Neutrophil-to-lymphocyte ratio as a quick and reliable predictive marker to diagnose the severity of diabetic retinopathy. Diabetes Technol Ther. 2013 Nov;15(11):942-7. doi: 10.1089/dia.2013.0097. Epub 2013 Aug 6. PMID: 23919588.
56. Dursun A, Ozturk S, Yucel H, Ozec AV, Dursun FG, Toker MI, Erdogan H, Arici MK, Topalkara A. Association of neutrophil/lymphocyte ratio and retinal vein occlusion. Eur J Ophthalmol. 2015 Jul-Aug;25(4):343-6. doi: 10.5301/ejo.5000570. Epub 2015 Jan 27. PMID: 25633622.
57. Celik T. Assessment of Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio in Patients with Dry Eye Disease. Ocul Immunol Inflamm. 2018;26(8):1219-1222. doi: 10.1080/09273948.2017.1340486. Epub 2017 Sep 14. PMID: 28910561.
58. Hanafi FD, Esa T, Nurulita A, Mumang AA. D-Dimer, ferritin, and lactate dehydrogenase (LDH) as predictors of mortality in hospitalized COVID-19 patients. J Infect Dev Ctries. 2024 Sep 30;18(9.1):S27-S32. doi: 10.3855/jidc.18833. PMID: 39499744.
59. Shama, Mahmood A, Mehmood S, Zhang W. Pathological Effects of SARS-CoV-2 Associated with Hematological Abnormalities. Curr Issues Mol Biol. 2023 Aug 28;45(9):7161-7182. doi: 10.3390/cimb45090453. PMID: 37754237; PMCID: PMC10528388.
2. Acharya S, Diamond M, Anwar S, Glaser A, Tyagi P. Unique case of central retinal artery occlusion secondary to COVID-19 disease. IDCases. 2020;21:e00867. doi: 10.1016/j.idcr.2020.e00867. Epub 2020 Jun 18. PMID: 32572363; PMCID: PMC7301806.
3. Insausti-García A, Reche-Sainz JA, Ruiz-Arranz C, López Vázquez Á, Ferro-Osuna M. Papillophlebitis in a COVID-19 patient: Inflammation and hypercoagulable state. Eur J Ophthalmol. 2022 Jan;32(1):NP168-NP172. doi: 10.1177/1120672120947591. Epub 2020 Jul 30. PMID: 32735134; PMCID: PMC7399568.
4. Landecho MF, Yuste JR, Gándara E, Sunsundegui P, Quiroga J, Alcaide AB, García-Layana A. COVID-19 retinal microangiopathy as an in vivo biomarker of systemic vascular disease? J Intern Med. 2021 Jan;289(1):116-120. doi: 10.1111/joim.13156. Epub 2020 Jul 30. PMID: 32729633.
5. Dumitrascu OM, Volod O, Bose S, Wang Y, Biousse V, Lyden PD. Acute ophthalmic artery occlusion in a COVID-19 patient on apixaban. J Stroke Cerebrovasc Dis. 2020 Aug;29(8):104982. doi: 10.1016/j.jstrokecerebrovasdis.2020.104982. Epub 2020 May 23. PMID: 32689586; PMCID: PMC7245224.
6. Ortiz-Seller A, Martínez Costa L, Hernández-Pons A, Valls Pascual E, Solves Alemany A, Albert-Fort M. Ophthalmic and Neuro-ophthalmic Manifestations of Coronavirus Disease 2019 (COVID-19). Ocul Immunol Inflamm. 2020 Nov 16;28(8):1285-1289. doi: 10.1080/09273948.2020.1817497. Epub 2020 Oct 6. PMID: 33021422.
7. Sanjay S, Srinivasan P, Jayadev C, Mahendradas P, Gupta A, Kawali A, Shetty R. Post COVID-19 Ophthalmic Manifestations in an Asian Indian Male. Ocul Immunol Inflamm. 2021 May 19;29(4):656-661. doi: 10.1080/09273948.2020.1870147. Epub 2021 Mar 18. PMID: 33733987.
8. Sanjay S, Gowda PB, Rao B, Mutalik D, Mahendradas P, Kawali A, Shetty R. "Old wine in a new bottle" - post COVID-19 infection, central serous chorioretinopathy and the steroids. J Ophthalmic Inflamm Infect. 2021 May 14;11(1):14. doi: 10.1186/s12348-021-00244-4. PMID: 33987731; PMCID: PMC8118683.
9. Sanjay S, Mutalik D, Gowda S, Mahendradas P, Kawali A, Shetty R. "Post Coronavirus Disease (COVID-19) Reactivation of a Quiescent Unilateral Anterior Uveitis". SN Compr Clin Med. 2021;3(9):1843-1847. doi: 10.1007/s42399-021-00985-2. Epub 2021 Jun 7. PMID: 34124585; PMCID: PMC8184259.
10. Sanjay S, Kawali A, Mahendradas P, Shetty B. Post Coronavirus Disease (COVID)-19 Disease and Unilateral Visual Impairment. Curr Eye Res. 2021 Dec;46(12):1938. doi: 10.1080/02713683.2021.1905001. Epub 2021 Mar 25. PMID: 33729900.
11. Mahendradas P, Hande P, Patil A, Kawali A, Sanjay S, Ahmed SA, Thomas S, Shetty R. Bilateral Post Fever Retinitis With Retinal Vascular Occlusions Following Severe Acute Respiratory Syndrome Corona Virus (SARS-CoV2) Infection. Ocul Immunol Inflamm. 2022 Oct-Nov;30(7-8):1715-1720. doi: 10.1080/09273948.2021.1936564. Epub 2021 Jul 6. PMID: 34228600.
12. Sanjay S, Agrawal S, Jayadev C, Kawali A, Gowda PB, Shetty R, Mahendradas P. Posterior segment manifestations and imaging features post-COVID-19. Med Hypothesis Discov Innov Ophthalmol. 2021 Nov 17;10(3):95-106. doi: 10.51329/mehdiophthal1427. PMID: 37641707; PMCID: PMC10460223.
13. Sanjay S, Rao VK, Mutalik D, Mahendradas P, Kawali A, Shetty R. Post corona virus Disease-19 (COVID-19): Hyper inflammatory syndrome-associated bilateral anterior uveitis and multifocal serous retinopathy secondary to steroids. Indian Journal of Rheumatology. 2021 Oct 1;16(4):451-5. doi: 10.4103/injr.injr_330_20.
14. Sanjay S, Singh YP, Roy D, Mahendradas P, Kawali A, Shetty R. Recurrent bilateral idiopathic anterior uveitis with vitritis post Coronavirus Disease 2019 infection. Indian Journal of Rheumatology. 2021 Dec;16(4):460-3. doi: 10.4103/injr.injr_114_21.
15. Sanjay S, Kawali A, Agrawal S, Mahendradas P. Unilateral acute anterior sclero-uveitis preceding Corona virus disease (COVID-19). The Pan-American Journal of Ophthalmology. 2022 Jan 1;4(1):26. doi: 10.4103/pajo.pajo_14_22.
16. Sanjay S, Bhakti Mistra S, Patro SK, Kawali A, Shetty R, Mahendradas P. Systemic Markers in Ophthalmic Manifestations of Post Corona Virus Disease-19 (COVID-19). Ocul Immunol Inflamm. 2023 Feb;31(2):410-415. doi: 10.1080/09273948.2021.2025253. Epub 2022 Feb 9. PMID: 35138993.
17. Sanjay S, Poornachandra B, Kawali A, Shetty R, Narayana VC, Agrawal S, Mahendradas P. Unilateral Endogenous Bacterial Endophthalmitis Post-Coronavirus Disease-19 in an Healthy Asian Indian Male. Beyoglu Eye J. 2022 Aug 5;7(3):240-246. doi: 10.14744/bej.2022.94546. PMID: 36185987; PMCID: PMC9522998.
18. Jabs DA, Nussenblatt RB, Rosenbaum JT; Standardization of Uveitis Nomenclature (SUN) Working Group. Standardization of uveitis nomenclature for reporting clinical data. Results of the First International Workshop. Am J Ophthalmol. 2005 Sep;140(3):509-16. doi: 10.1016/j.ajo.2005.03.057. PMID: 16196117; PMCID: PMC8935739.
19. Nussenblatt RB, Palestine AG, Chan CC, Roberge F. Standardization of vitreal inflammatory activity in intermediate and posterior uveitis. Ophthalmology. 1985 Apr;92(4):467-71. doi: 10.1016/s0161-6420(85)34001-0. PMID: 4000641.
20. Forget P, Khalifa C, Defour JP, Latinne D, Van Pel MC, De Kock M. What is the normal value of the neutrophil-to-lymphocyte ratio? BMC Res Notes. 2017 Jan 3;10(1):12. doi: 10.1186/s13104-016-2335-5. PMID: 28057051; PMCID: PMC5217256.
21. Arabska J, ?ucka A, Magierski R, Sobów T, Wysoki?ski A. Neutrophil-lymphocyte ratio is increased in elderly patients with first episode depression, but not in recurrent depression. Psychiatry Res. 2018 May;263:35-40. doi: 10.1016/j.psychres.2018.02.043. Epub 2018 Feb 21. PMID: 29490259.
22. Prokop M, van Everdingen W, van Rees Vellinga T, Quarles van Ufford H, Stöger L, Beenen L, Geurts B, Gietema H, Krdzalic J, Schaefer-Prokop C, van Ginneken B, Brink M; COVID-19 Standardized Reporting Working Group of the Dutch Radiological Society. CO-RADS: A Categorical CT Assessment Scheme for Patients Suspected of Having COVID-19-Definition and Evaluation. Radiology. 2020 Aug;296(2):E97-E104. doi: 10.1148/radiol.2020201473. Epub 2020 Apr 27. PMID: 32339082; PMCID: PMC7233402.
23. Elmokadem AH, Mounir AM, Ramadan ZA, Elsedeiq M, Saleh GA. Comparison of chest CT severity scoring systems for COVID-19. Eur Radiol. 2022 May;32(5):3501-3512. doi: 10.1007/s00330-021-08432-5. Epub 2022 Jan 15. PMID: 35031841; PMCID: PMC8760133.
24. Merli G, Spiro TE, Olsson CG, Abildgaard U, Davidson BL, Eldor A, Elias D, Grigg A, Musset D, Rodgers GM, Trowbridge AA, Yusen RD, Zawilska K; Enoxaparin Clinical Trial Group. Subcutaneous enoxaparin once or twice daily compared with intravenous unfractionated heparin for treatment of venous thromboembolic disease. Ann Intern Med. 2001 Feb 6;134(3):191-202. doi: 10.7326/0003-4819-134-3-200102060-00009. PMID: 11177331.
25. Cerfolio RJ, Bryant AS, Thurber JS, Bass CS, Lell WA, Bartolucci AA. Intraoperative solumedrol helps prevent postpneumonectomy pulmonary edema. Ann Thorac Surg. 2003 Oct;76(4):1029-33; discussion 1033-5. doi: 10.1016/s0003-4975(03)00879-8. PMID: 14529979.
26. Billett HH, Reyes-Gil M, Szymanski J, Ikemura K, Stahl LR, Lo Y, Rahman S, Gonzalez-Lugo JD, Kushnir M, Barouqa M, Golestaneh L, Bellin E. Anticoagulation in COVID-19: Effect of Enoxaparin, Heparin, and Apixaban on Mortality. Thromb Haemost. 2020 Dec;120(12):1691-1699. doi: 10.1055/s-0040-1720978. Epub 2020 Nov 13. PMID: 33186991; PMCID: PMC7869055.
27. Bikdeli B, Madhavan MV, Jimenez D, Chuich T, Dreyfus I, Driggin E, Nigoghossian C, Ageno W, Madjid M, Guo Y, Tang LV, Hu Y, Giri J, Cushman M, Quéré I, Dimakakos EP, Gibson CM, Lippi G, Favaloro EJ, Fareed J, Caprini JA, Tafur AJ, Burton JR, Francese DP, Wang EY, Falanga A, McLintock C, Hunt BJ, Spyropoulos AC, Barnes GD, Eikelboom JW, Weinberg I, Schulman S, Carrier M, Piazza G, Beckman JA, Steg PG, Stone GW, Rosenkranz S, Goldhaber SZ, Parikh SA, Monreal M, Krumholz HM, Konstantinides SV, Weitz JI, Lip GYH; Global COVID-19 Thrombosis Collaborative Group, Endorsed by the ISTH, NATF, ESVM, and the IUA, Supported by the ESC Working Group on Pulmonary Circulation and Right Ventricular Function. COVID-19 and Thrombotic or Thromboembolic Disease: Implications for Prevention, Antithrombotic Therapy, and Follow-Up: JACC State-of-the-Art Review. J Am Coll Cardiol. 2020 Jun 16;75(23):2950-2973. doi: 10.1016/j.jacc.2020.04.031. Epub 2020 Apr 17. PMID: 32311448; PMCID: PMC7164881.
28. Bapaye MM, Nair AG, Bapaye CM, Bapaye MM, Shukla JJ. Simultaneous Bilateral Central Retinal Artery Occlusion following COVID-19 Infection. Ocul Immunol Inflamm. 2021 May 19;29(4):671-674. doi: 10.1080/09273948.2021.1891262. Epub 2021 Apr 15. PMID: 33856275.
29. Erdem S, Karahan M, Dursun ME, Ava S, Hazar L, Katran I, Keklikci U. Retinal Vasculitis Case Developing in the Early Period after COVID-19. Klin Monbl Augenheilkd. 2022 Sep;239(9):1132-1133. English. doi: 10.1055/a-1363-1326. Epub 2021 Apr 14. PMID: 33853180.
30. Seah I, Agrawal R. Can the Coronavirus Disease 2019 (COVID-19) Affect the Eyes? A Review of Coronaviruses and Ocular Implications in Humans and Animals. Ocul Immunol Inflamm. 2020 Apr 2;28(3):391-395. doi: 10.1080/09273948.2020.1738501. Epub 2020 Mar 16. PMID: 32175797; PMCID: PMC7103678.
31. Hooks JJ, Percopo C, Wang Y, Detrick B. Retina and retinal pigment epithelial cell autoantibodies are produced during murine coronavirus retinopathy. J Immunol. 1993 Sep 15;151(6):3381-9. PMID: 8397257.
32. Becker RC. COVID-19 update: Covid-19-associated coagulopathy. J Thromb Thrombolysis. 2020 Jul;50(1):54-67. doi: 10.1007/s11239-020-02134-3. PMID: 32415579; PMCID: PMC7225095.
33. Sen S, Kannan NB, Kumar J, Rajan RP, Kumar K, Baliga G, Reddy H, Upadhyay A, Ramasamy K. Retinal manifestations in patients with SARS-CoV-2 infection and pathogenetic implications: a systematic review. Int Ophthalmol. 2022 Jan;42(1):323-336. doi: 10.1007/s10792-021-01996-7. Epub 2021 Aug 11. PMID: 34379290; PMCID: PMC8356207.
34. Tao DL, Bien JY, DeLoughery TG, Shatzel JJ. Extended thromboprophylaxis with direct oral anticoagulants for medical patients: a systematic review and meta-analysis. Blood. 2017 Feb 2;129(5):653-655. doi: 10.1182/blood-2016-10-747931. Epub 2016 Dec 20. PMID: 27998890.
35. Pinto AA, Carroll LS, Nar V, Varatharaj A, Galea I. CNS inflammatory vasculopathy with antimyelin oligodendrocyte glycoprotein antibodies in COVID-19. Neurol Neuroimmunol Neuroinflamm. 2020 Jun 10;7(5):e813. doi: 10.1212/NXI.0000000000000813. PMID: 32522768; PMCID: PMC7309522.
36. Roncati L, Ligabue G, Fabbiani L, Malagoli C, Gallo G, Lusenti B, Nasillo V, Manenti A, Maiorana A. Type 3 hypersensitivity in COVID-19 vasculitis. Clin Immunol. 2020 Aug;217:108487. doi: 10.1016/j.clim.2020.108487. Epub 2020 May 29. PMID: 32479986; PMCID: PMC7256503.
37. Xie CA, Singh J, Tyagi M, Androudi S, Dave VP, Arora A, Gupta V, Agrawal R, Mi H, Sen A. Endogenous Endophthalmitis - A Major Review. Ocul Immunol Inflamm. 2023 Sep;31(7):1362-1385. doi: 10.1080/09273948.2022.2126863. Epub 2022 Oct 28. PMID: 36306406.
38. Cunningham ET, Flynn HW, Relhan N, Zierhut M. Endogenous Endophthalmitis. Ocul Immunol Inflamm. 2018;26(4):491-495. doi: 10.1080/09273948.2018.1466561. PMID: 29768116; PMCID: PMC6448583.
39. Ren C, Li Z, Meng F, Du Y, Sun H, Guo B. Endogenous endophthalmitis caused by urinary tract infection: A case report. Medicine (Baltimore). 2023 Nov 17;102(46):e36139. doi: 10.1097/MD.0000000000036139. PMID: 37986372; PMCID: PsMC10659675.
40. Shroff D, Narula R, Atri N, Chakravarti A, Gandhi A, Sapra N, Bhatia G, Pawar SR, Narain S. Endogenous fungal endophthalmitis following intensive corticosteroid therapy in severe COVID-19 disease. Indian J Ophthalmol. 2021 Jul;69(7):1909-1914. doi: 10.4103/ijo.IJO_592_21. PMID: 34146056; PMCID: PMC8374784.
41. Obata R, Maeda T, Rizk D, Kuno T. Increased Secondary Infection in COVID-19 Patients Treated with Steroids in New York City. Jpn J Infect Dis. 2021 Jul 21;74(4):307-315. doi: 10.7883/yoken.JJID.2020.884. Epub 2020 Dec 25. PMID: 33390434.
42. Agarwal M, Sachdeva M, Pal S, Shah H, Kumar R M, Banker A. Endogenous Endophthalmitis A Complication of COVID-19 Pandemic: A Case Series. Ocul Immunol Inflamm. 2021 May 19;29(4):726-729. doi: 10.1080/09273948.2021.1945111. Epub 2021 Jul 13. PMID: 34255587.
43. Bilgic A, Sudhalkar A, Gonzalez-Cortes JH, March de Ribot F, Yogi R, Kodjikian L, Mathis T. ENDOGENOUS ENDOPHTHALMITIS IN THE SETTING OF COVID-19 INFECTION: A Case Series. Retina. 2021 Aug 1;41(8):1709-1714. doi: 10.1097/IAE.0000000000003168. PMID: 33734193.
44. Verma S, Walinjkar JA. A case of endogenous endophthalmitis in COVID-19 pandemic. Apollo Medicine. 2020 Sep;17(3):229-32. doi: https://journals.sagepub.com/doi/abs/10.4103/am.am_71_20.
45. Shah KK, Venkatramani D, Majumder PD. A case series of presumed fungal endogenous endophthalmitis in post COVID-19 patients. Indian J Ophthalmol. 2021 May;69(5):1322-1325. doi: 10.4103/ijo.IJO_3755_20. PMID: 33913891; PMCID: PMC8186646.
46. Khatwani PR, Goel NP, Trivedi KY, Aggarwal SV. Unveiling endophthalmitis post COVID-19 - A case series. Indian J Ophthalmol. 2021 Oct;69(10):2869-2871. doi: 10.4103/ijo.IJO_1616_21. PMID: 34571655; PMCID: PMC8597453.
47. Abdelkader MFSO, Elshafei AMK, Nassar MM, Abu Elela MA, Abdallah RMA. Combined endophthalmitis and orbital cellulitis in patients with corona virus disease (COVID-19). J Ophthalmic Inflamm Infect. 2021 Sep 15;11(1):27. doi: 10.1186/s12348-021-00258-y. PMID: 34523045; PMCID: PMC8440116.
48. Jain M, Brar AS, Rath S, Kelgaokar A, Behera HS. Fulminant fungal endogenous endophthalmitis following SARS-CoV-2 infection: A case report. Indian J Ophthalmol. 2022 May;70(5):1819-1821. doi: 10.4103/ijo.IJO_1951_21. PMID: 35502083; PMCID: PMC9333037.
49. Deepa MJ, Megharaj C, Patil S, Rani PK. Cryptococcus laurentii endogenous endophthalmitis post COVID-19 infection. BMJ Case Rep. 2022 May 11;15(5):e246637. doi: 10.1136/bcr-2021-246637. PMID: 35545307; PMCID: PMC9096502.
50. Sahu ES, Lahoti K, Bhargava A, Subhedar V, Sahu A. Subretinal Aspergillus Abscess in Post COVID-19 Recovered Patients - An Emerging Problem. Ocul Immunol Inflamm. 2023 Jan;31(1):127-133. doi: 10.1080/09273948.2021.1993271. PMID: 34784260.
51. Song M, Graubard BI, Rabkin CS, Engels EA. Neutrophil-to-lymphocyte ratio and mortality in the United States general population. Sci Rep. 2021 Jan 11;11(1):464. doi: 10.1038/s41598-020-79431-7. PMID: 33431958; PMCID: PMC7801737.
52. Kurtul BE, Ozer PA. Neutrophil-to-lymphocyte ratio in ocular diseases: a systematic review. Int J Ophthalmol. 2019 Dec 18;12(12):1951-1958. doi: 10.18240/ijo.2019.12.18. PMID: 31850181; PMCID: PMC6901879.
53. Ozgonul C, Sertoglu E, Mumcuoglu T, Kucukevcilioglu M. Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio as Novel Biomarkers of Primary Open-Angle Glaucoma. J Glaucoma. 2016 Oct;25(10):e815-e820. doi: 10.1097/IJG.0000000000000392. PMID: 26918914.
54. Chittawar S, Dutta D, Qureshi Z, Surana V, Khandare S, Dubey TN. Neutrophil-lymphocyte Ratio is a Novel Reliable Predictor of Nephropathy, Retinopathy, and Coronary Artery Disease in Indians with Type-2 Diabetes. Indian J Endocrinol Metab. 2017 Nov-Dec;21(6):864-870. doi: 10.4103/ijem.IJEM_197_17. PMID: 29285450; PMCID: PMC5729675.
55. Ulu SM, Dogan M, Ahsen A, Altug A, Demir K, Acartürk G, Inan S. Neutrophil-to-lymphocyte ratio as a quick and reliable predictive marker to diagnose the severity of diabetic retinopathy. Diabetes Technol Ther. 2013 Nov;15(11):942-7. doi: 10.1089/dia.2013.0097. Epub 2013 Aug 6. PMID: 23919588.
56. Dursun A, Ozturk S, Yucel H, Ozec AV, Dursun FG, Toker MI, Erdogan H, Arici MK, Topalkara A. Association of neutrophil/lymphocyte ratio and retinal vein occlusion. Eur J Ophthalmol. 2015 Jul-Aug;25(4):343-6. doi: 10.5301/ejo.5000570. Epub 2015 Jan 27. PMID: 25633622.
57. Celik T. Assessment of Neutrophil-to-Lymphocyte Ratio and Platelet-to-Lymphocyte Ratio in Patients with Dry Eye Disease. Ocul Immunol Inflamm. 2018;26(8):1219-1222. doi: 10.1080/09273948.2017.1340486. Epub 2017 Sep 14. PMID: 28910561.
58. Hanafi FD, Esa T, Nurulita A, Mumang AA. D-Dimer, ferritin, and lactate dehydrogenase (LDH) as predictors of mortality in hospitalized COVID-19 patients. J Infect Dev Ctries. 2024 Sep 30;18(9.1):S27-S32. doi: 10.3855/jidc.18833. PMID: 39499744.
59. Shama, Mahmood A, Mehmood S, Zhang W. Pathological Effects of SARS-CoV-2 Associated with Hematological Abnormalities. Curr Issues Mol Biol. 2023 Aug 28;45(9):7161-7182. doi: 10.3390/cimb45090453. PMID: 37754237; PMCID: PMC10528388.
- Abstract Viewed: 0 times
- Full Text PDF Downloaded: 0 times